Let’s face it, placing our health in the hands of medical professionals requires immense trust. When that trust is broken, and you suffer harm due to substandard care, the question of medical malpractice arises. But what exactly is it, and how do you know if you have a valid claim? This article aims to demystify the often-complex world of medical negligence.
1. Understanding Medical Malpractice: A Necessary Introduction
Medical malpractice, also often referred to as clinical negligence, occurs when a healthcare provider’s actions or omissions fall below the accepted standard of care, resulting in injury to a patient. It’s not simply about an unfavourable outcome; it’s about negligent behaviour that directly leads to harm. Understanding the nuances is crucial before considering legal action.
2. Defining Medical Malpractice: Key Elements and Legal Standards
To successfully claim medical malpractice, several key elements must be proven. Legally, you generally need to demonstrate these four things:
- Duty of Care: A doctor-patient relationship must exist, establishing the doctor’s responsibility to provide care. This is usually straightforward, but can be complicated if, for example, the doctor offered informal advice outside of a formal consultation.
- Breach of Duty: The healthcare provider must have deviated from the accepted “standard of care.” This means they acted in a way that another reasonably competent healthcare professional in the same specialty wouldn’t have under similar circumstances.
- Causation: A direct link must be established between the breach of duty and the patient’s injury. It’s not enough to show negligence; you must prove it caused the harm.
- Damages: The patient must have suffered actual damages as a result of the injury, such as physical pain, emotional distress, lost income, and medical expenses.
The “standard of care” is pivotal. What is considered acceptable practice varies based on the specific medical field, the resources available, and even geographical location.
3. What Can Be Considered Medical Malpractice: Common Examples and Scenarios
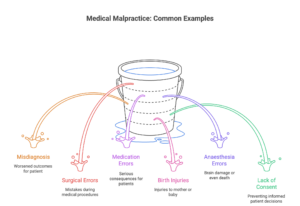
Examples of what can be considered clinical negligence are varied:
- Misdiagnosis or Delayed Diagnosis: Failing to accurately diagnose a condition or delaying diagnosis can lead to worsened outcomes. A recent case in London involved a delayed diagnosis of cancer due to misinterpreting scan results, resulting in a less favourable prognosis for the patient.
- Surgical Errors: Mistakes during surgery, such as operating on the wrong site or leaving instruments inside the body, are clear examples.
- Medication Errors: Prescribing the wrong medication, incorrect dosage, or failing to consider drug interactions can have serious consequences.
- Birth Injuries: Negligence during childbirth can cause injuries to the mother or the baby, such as cerebral palsy or Erb’s palsy.
- Anaesthesia Errors: Errors in administering anaesthesia can lead to brain damage or even death.
- Failure to Obtain Informed Consent: Performing a procedure without properly explaining the risks and benefits, thus preventing the patient from making an informed decision.
Recent data from NHS Resolution (the organisation that handles medical negligence claims in England) shows that claims related to surgical errors and delays in diagnosis continue to be significant drivers of compensation payouts.
4. Beyond Negligence: Establishing Causation in Medical Malpractice Cases
Proving that the doctor’s negligence directly caused your injury is often the most challenging aspect of a medical malpractice case. Expert witnesses play a crucial role here. They can provide testimony explaining the medical aspects of the case and how the doctor’s actions (or lack thereof) caused the patient’s harm.
For instance, imagine a patient experiences a stroke after surgery. To win a malpractice claim, they’d need to prove the stroke was directly caused by the surgeon’s negligence, rather than pre-existing conditions or other factors. Medical experts would need to testify explaining the connection.
5. What Doesn’t Qualify as Medical Malpractice: Unsuccessful Treatment vs. Negligence
Not every bad outcome constitutes medical malpractice. Sometimes, treatment is unsuccessful despite the doctor providing competent care. Medicine isn’t an exact science, and complications can arise even when everything is done correctly. For example, a patient might not respond to a prescribed medication, or a surgery might not achieve the desired result, even if the doctor followed all proper procedures.
A crucial difference lies between a known risk of a procedure (which the patient was informed about) and negligence that directly caused the problem. Simply disliking your doctor isn’t grounds for a case either.
6. Pursuing a Medical Malpractice Claim: Essential Steps and Considerations
If you believe you have a valid claim, there are key steps to take:
- Seek Legal Advice: Consult with a solicitor experienced in medical negligence. They can assess your case’s viability and guide you through the legal process.
- Gather Medical Records: Obtain copies of all relevant medical records, including doctor’s notes, test results, and hospital records.
- Investigate: Your solicitor will investigate the case, often involving expert medical review to determine if the standard of care was breached.
- File a Claim: If the investigation supports your claim, your solicitor will file a formal claim against the healthcare provider or their insurance company.
- Negotiation or Litigation: The claim may be settled through negotiation, mediation, or arbitration. If a settlement cannot be reached, the case may proceed to court.
Statute of Limitations: Be aware of the statute of limitations, which sets a time limit for filing a claim. In the UK, this is generally three years from the date of the negligent act or the date you became aware of the injury. However, exceptions exist, such as for children or those lacking mental capacity.
Alternative Dispute Resolution: Options such as mediation and arbitration offer a less adversarial and often quicker path to resolving disputes compared to going to court. These methods involve a neutral third party who helps facilitate a settlement.
Insurance and Liability: Doctors and hospitals typically carry professional liability insurance to cover potential medical malpractice claims. Claims are usually handled by the insurance company, which will investigate the claim and defend the healthcare provider.
7. Preventing Medical Malpractice: A Shared Responsibility
While patients have rights, preventing clinical negligence is a shared responsibility. Healthcare providers must be diligent in their practices, stay up-to-date with medical advancements, and prioritise patient safety. Hospitals and clinics need robust systems for reporting and addressing errors. Patients, too, can play a role by being proactive in their care, asking questions, and providing complete medical histories.
Ethical Considerations: Medical professionals face a complex web of ethical obligations. Potential conflicts of interest, such as financial incentives or pressure from superiors, can sometimes compromise patient care. Transparency and a commitment to ethical conduct are crucial to maintaining trust and preventing malpractice.
Ultimately, understanding what constitutes clinical negligence is vital for both patients and healthcare professionals. It ensures accountability, promotes safer medical practices, and allows those harmed by negligence to seek justice and compensation for their injuries.





